Find out more about filaggrin
Dr George Moncrieff introduces a skin protein that is vital for skin health – but is impaired in more than half of people with eczema. This article was published in Exchange 177, September 2020.
If you have atopic eczema, you really need to know about filaggrin. This large protein was first discovered by Beverly A. Dale, back in 1977. However it was not until 2006 that its critical role in developing the skin barrier was described by a remarkable geneticist from Dundee, called Professor Irwin McLean.
The skin structure
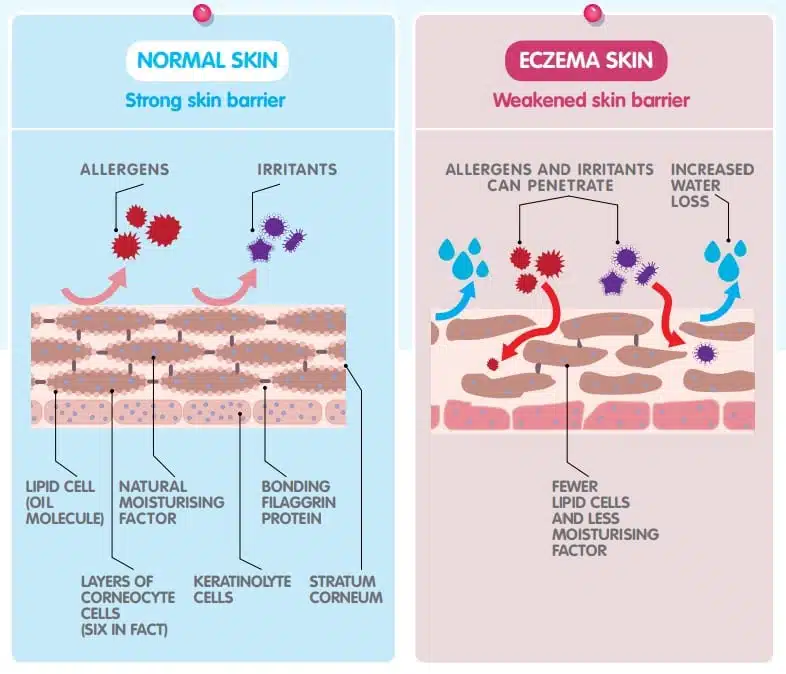
The outer layer of our skin is the epidermis. This is essentially made up of four layers. The outer one is called the stratum corneum and that is the skin barrier. In some parts of the body – for example, the eyelid – the stratum corneum is one-tenth as thick as a piece of paper and is therefore very vulnerable.
The cells in this layer have no nuclei, so some people in their ignorance describe these as ‘dead cells waiting to fall off’. For ‘dead cells’, they are astonishingly clever. They are no more ‘dead’, though, than the red cells in our bloodstream, which also have no nuclei. The layer of cells just below the stratum corneum is called the stratum granulosa – so called as two important types of granule develop in the cytoplasm of these cells.
The first is lipid lamella granules, which produce a number of fatty substances, including ceramides (also added to some sophisticated emollients). This forms an oily ‘cement’ around the cells in the stratum corneum, sealing the spaces between the cells and conferring elasticity to the skin.
The other granules in this layer produce tonofilaments: keratin rods within the cell, rather like steel rods in reinforced concrete. They also produce profilaggrin – an enormous protein that rapidly breaks down into filaggrin.
What filaggrin does
Filaggrin’s first function is to aggregate the tonofilaments, hence its name: filament aggregating protein. As the filaments are aggregated, they form into a lattice-like structure. When this reaches a critical size, it collapses on itself, rather like an ironing board being put away. This dramatically changes the shape of the cell, from the cuboidal shape in the stratum granulosa to the flattened, stratified shape of the cells in the stratum corneum.
These flat cells have a huge surface area, which enables easy bonding to their neighbours. It also offers considerable overlap and is therefore a more effective barrier to water loss or ingression of allergens or pathogens such as bacteria or viruses.
Once this shape change has been achieved, the filaggrin itself is broken down into multiple small molecules: amino acids, urocanic acid, pyrollidine carboxylic acid, uric acid, lactic acid, along with many others.
These small molecules are all extremely hygroscopic – in other words, they draw water molecules to them and retain that moisture. That hydrates the cells in the stratum corneum, making the cells bulge so they are pushed up hard against one another, further enhancing the barrier.
They are all also acids as well and form a fundamental part of the essential ‘acid mantle’ on the surface of the skin. Without filaggrin and these breakdown products, the normal acidic pH of the skin (pH4.5) could not be achieved.
This acid mantle is crucial as it controls the activity of the enzymes that break down the bonds that hold the cells in stratum corneum together. It also has natural antibacterial activity as well as enhancing the non-pathogenic ‘healthy’ bacteria.
What does this mean for eczema?
Perversely, once the skin has become inflamed (from eczema, for example), the granular activity in stratum granulosa is switched off, making the skin barrier all the more vulnerable and creating a vicious cycle. Furthermore, one of my many concerns about topical steroids is that they also de-granulate the stratum granulosa and are therefore not ideal for long-term use, as production of ceramides, the tonofilaments and profilaggrin (as well as many other critical substances) is reduced.
Eczema occurs where the skin is the most thin and the skin barrier is the weakest. Protecting these weak areas is an essential part of eczema management.
Genetic factors
There is an important gene complex on Chromosome 1 called the epidermal differentiation gene. This gene complex codes for the lipid lamella granules. It controls the production of the proteases (enzymes) that break down the corneodesmosomes – the strong bonds between the cells in the stratum corneum. It also codes for the production of desmosin – the enzyme that converts the weaker desmosomes in the stratum granulosa into the strong corneodesmosomes. Finally, it codes for the filaments and profilaggrin.
In about 10% of our population, this gene is faulty. This results in reduced production of normal filaggrin. And this gene is faulty in more than 50% of people with atopic dermatitis.
The epidermal differentiation gene is faulty in more than 50% of people with atopic dermatitis.
Today, we believe that the reason this gene fault is so common is because in our ancestors it resulted in a weakness in the skin barrier, making an individual more likely to be exposed to cowpox virus. In the days when smallpox was rife, causing large numbers of deaths, this ‘natural vaccination’ against the pox family conferred considerable advantages.
Today, cowpox and smallpox are no longer concerns, but the gene has persisted. However, our modern lifestyle, with over-washing and fanatical overuse of detergents (such as shower gels, soaps and shampoos) on our skin, exposes this barrier weakness and causes eczema.
Complete loss of filaggrin gene activity results in a condition called ichthyosis vulgaris (which literally means ‘very common, fish-like scale’). This is indeed common, affecting around 2% of the population, but is rarely diagnosed. This is because, while these individuals have remarkably dry, uncomfortable skin, strangely it is not especially itchy and not all people with this develop atopic eczema.
Clearly, there is even more to the extraordinary functions of the stratum corneum than is currently understood.
The development of a skin barrier is a remarkable piece of genetic evolution and quite astonishingly sophisticated. It protects our inner sterile, healthy environment from the hostile world we all live in, even when it is just one-tenth as thick as a piece of paper – all the more remarkable for ‘dead cells’! Our modern lifestyle rips into that, exposing the weakness that might otherwise be innocuous.
