Mental health support
Jump to:
Habit reversal and the combined approach
Could CBT help me cope with eczema?
The experience of living with eczema can take its toll. Cognitive behavioural therapy (CBT) is an evidence-based therapy that could make a difference. Dr Alpa Kanji tells us more. This article was published in Exchange 186, Winter 2022.
Living with eczema can be very challenging. The physical impact of living with the condition can be very difficult to cope with: the constant sensation of itch, subsequent scratching, unpredictable flares, painful broken skin and disturbed sleep. People living with eczema also report the wider negative effect on their daily activities including personal relationships, work and social lives. The visibility of eczema can also bring feelings of embarrassment, shame, low confidence and loneliness.
The impact of all these challenges on wellbeing can be significant and long term, so psychological support is important. Cognitive behavioural therapy (CBT) is one option that can help.
What is CBT?
CBT is a talking therapy often used to help people with anxiety and depression. Evidence shows it can also help people living with long-term health conditions, such as eczema, as well as associated problems, such as sleep difficulties, stress, anger and low self-esteem. It can be helpful for adults as well as children and young people.
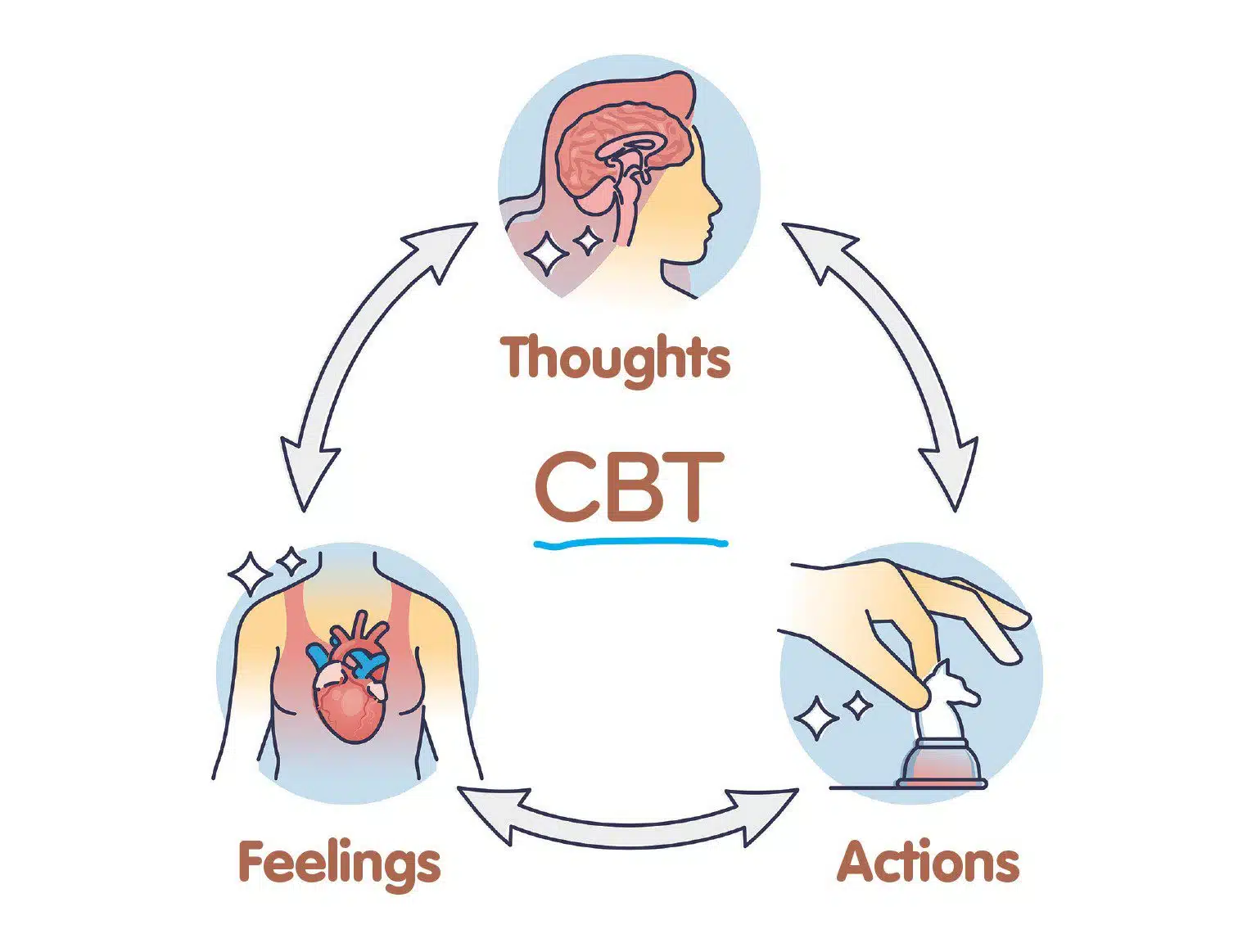
CBT is based on the idea that thoughts, feelings and actions are all interrelated and that changing one ‘link in the chain’ can impact the others. An important part of CBT is learning new, more balanced ways of thinking and doing, to help you cope better with challenging problems. Working alongside a therapist, problems can be broken down into more manageable chunks.
The ‘C’ stands for ‘cognitive’ – this involves learning to notice your thought patterns and identify any that are unhelpful or unrealistic, to develop more useful ways of thinking.
The ‘B’ stands for ‘behavioural’, which refers to the actions you take. You learn to identify and replace unhelpful actions and behaviours with better ones. For someone with eczema, this may mean learning strategies to reduce scratching in certain situations or building up a consistent skin-care regime.
CBT might help to address wider behaviours too – for example, some people feel so embarrassed about their visible eczema that they avoid going out. It can also help people accept the reality of living with eczema and dealing with unpredictable flares.
The process involves working with a trained therapist during a series of sessions, over weeks or months. At the outset, you both agree on what you are trying to achieve and the process is tailored to the person’s individual circumstances. CBT focuses mainly on improving your mental wellbeing in the present, to help you to feel better and create a more positive future.
To help you practise these skills in daily life, so that you can learn to apply them to everyday situations, the therapist assigns ‘homework’. This may involve activities such as journalling, learning to critically evaluate your thoughts and being able to challenge your actions. The therapist works with you to review your homework in the sessions and monitor your progress.
CBT takes time and commitment as well as gradual practice, to replace old ways of doing things with new ones. Where it is successful, it can help people to cope better with living with eczema, resulting in long-term benefits and a more positive outlook on life.
Does it work?
CBT has been shown to help people face a range of challenges by helping them overcome negative thoughts and emotions and unhelpful behaviours. There is also evidence that CBT can help people better manage life with eczema, by reducing anxiety and depression and stigmatising beliefs.
What does the research say?
In 2021, 102 adults with eczema took part in a study in Sweden that involved receiving internet-based CBT for 12 weeks. They were compared to a group of people who received education about their condition but no therapy. By the end of the trial, the people who received CBT had less intense itching, reduced stress levels, better sleep and fewer symptoms of depression at the end.
How do I access CBT?
CBT is available in several different formats, including face to face, by phone and online.
GP referral If eligible, your GP can refer to local CBT services on the NHS.
IAPT (the Improved Access to Psychological Therapies programme) is a programme providing CBT in England. This does not require a GP referral, although you need to be registered with a GP to access the service.
Dermatology referral Larger dermatology centres in the UK may have psychological services available to patients with chronic skin conditions but at present these are limited. If you have a dermatologist, they may be able to refer you for CBT where this service is available.
Children and young people can access CBT through Children and Adolescent Mental Health Services (CAMHS), through a GP referral, although there may be long waiting lists.
Private therapists You can also access a therapist privately. This involves paying for the sessions. The British Association of Behavioural and Cognitive Psychotherapies (BABCP) has a register of all the accredited therapists in the UK who have met required standards. Visit its website to find one in your area.
What else might help?
If you can’t access CBT easily, or if there is a delay, there are other things that might be helpful:
Self-help CBT resources are available in book form or online (such as the websites Getselfhelp and Living Life to the Full).
Talk about it to a close friend or trusted family member.
Share your experiences of living with eczema with people who understand – for example, on an online forum or through an organisation such as National Eczema Society or Eczema Outreach Support.
Learn relaxation techniques As stress can often exacerbate eczema, learning strategies to better manage this, including relaxation techniques, can be helpful. There are several online resources that might help with this.
Find out more
- NHS support on mental health
- Online CBT self-help resources: Getselfhelp and Living Life to the Full
- British Association of Behavioural and Cognitive Psychotherapists
- Eczema Outreach Support
- Online guide to managing stress
Dr Alpa Kanji is a dermatologist at West Hertfordshire Teaching Hospitals NHS Trust. She has a particular interest in atopic dermatitis and is passionate about empowering patients to manage their skin condition.
Habit Reversal and the Combined Approach
An approach that combines behavioural modification with optimised topical treatment is helping people break the cycle of scratching and get on top of their eczema flares. Dr Alpa Kanji explains how it works. This article was published in Exchange 178, December 2020.
Eczema can be a highly distressing condition to live with. The psychological burden of living with a chronic skin condition may be substantial, causing feelings of social isolation, embarrassment and low confidence. Even its physical effects – itchiness, sleep disturbance, sore, broken skin resulting from scratching – take their toll on people’s emotional well-being.
The problem with scratching
A key feature of eczema is the itch. It is understandable that many people respond to this by scratching, picking or rubbing the skin to get relief. However over time, this scratching behaviour can become generalised and habitual. The person then starts scratching in response to other stimuli such as stress, tiredness and even boredom – often without being aware of what they are doing.
The mainstays of eczema treatment are emollients and topical steroid creams.
Emollients help to strengthen the skin barrier and reduce the dryness, while topical steroids have an anti-inflammatory effect on the skin. However, as long as there is habitual scratching, the skin never fully heals and the eczema persists.
This longstanding eczema is referred to as ‘chronic’ as it persists for weeks and months in contrast to the short-lived flares of eczema, which are ‘acute’. Chronic eczema can be recognised by thickened, leathery skin in easy-to-reach places. Once the habitual scratching is ‘switched off’, this skin returns to normal.
How habit reversal can help
To fully heal the skin and eradicate the chronic eczema, we need to address the habitual scratching and rubbing: enter habit reversal.
Habit reversal is a behaviour modification approach originally used by psychologists to successfully eradicate nervous habits such as hair pulling and nail biting. This technique was first adopted for people with eczema by Dr Peter Norén, a Swedish dermatologist. Habit reversal is simple and easy to learn and helps reduce scratching behaviour, allowing chronic eczema to heal.
The combined approach
When habit reversal is used alongside optimal topical therapy (in other words, steroids and emollients), this is known as the ‘combined approach’. This approach was first introduced to the UK in 1989 by doctors Richard Staughton and Christopher Bridgett and became established at London’s Chelsea and Westminster Hospital.
The combined approach typically involves a series of four-to-six consultations over two months. First, we help the person to develop an increased awareness of their scratching behaviour and associated stimuli by recording episodes of touching, scratching or picking the skin, using a tally counter. Then we teach them how to minimise the number of scratching episodes. Once the scratching stops, the skin can heal.
Active participation is an essential aspect of this programme: we teach the person how to help themselves and give them homework to do after each session. We monitor their progress through the tally counts, as they record the number of scratching episodes each day. These may start off ranging from 100 to 1,000 episodes per day. By the end of the programme, they should be substantially reduced.
Next, we optimise the person’s medication. We may prescribe stronger preparations for the short duration of the programme in a safe and supervised manner.
Does it work?
This simple technique has been shown to work. Several published studies have shown a reduction in chronic eczema when habit reversal is combined with optimal topical treatment, compared to topical treatment alone.
The combined approach can be very empowering as people begin to realise that their efforts have a direct, positive impact on their skin. This promotes attitudes of active optimism and self-help, which are important aspects of this programme.
Once the person has successfully completed the programme, we show them how to recognise and eradicate eczema flares quickly, by applying topical treatment correctly. We discuss their triggers for flare-ups and help them to separate those into ‘avoidable’ versus ‘unavoidable’. This makes it easier for them to manage acute eczema.
Over time, the number of acute relapses decreases and the period of remission between each episode becomes longer. Skin with a tendency for eczema can be dry, so the person may need to keep using emollients, but there is usually much less need for the ongoing routine use of topical steroids. Some find that the years of struggle with chronic eczema are replaced with eczema-free skin. This can have a profound effect on well-being, positively impacting many aspects of daily life.
Where is it available?
This programme is available to a limited number of adults and older children at the Chelsea and Westminster Hospital. It is also being offered at several centres in the UK but may not be readily available to everyone who may benefit from it. Former patient Sue Armstrong-Brown details each step of the programme in a self-help book entitled The Eczema Solution, which documents her journey and her experience of the programme.
Case Study: Ilaha Akhbar (19) describes the combined approach from a patient’s perspective.
I have had eczema since childhood and used many creams, ointments and stronger oral medications to try to control it. Most recently I was taking ciclosporin tablets but my eczema did not significantly improve and I was experiencing headaches so had to stop taking it.
I was due to be seen in clinic for consideration of dupilumab – a newer medication taken by injection. In the meantime, I was offered a clinic appointment to learn the combined approach and habit reversal. I was sceptical when I heard about this and thought it might be another series of ‘verbal’ appointments.
My first appointment did involve a lot of discussion. I learned the difference between ‘itch’ (a sensation) and ‘scratch’ (an action). Reducing the habitual scratching was a key aspect to breaking the itch–scratch cycle, which – along with intensive topical treatment – could eliminate the longstanding eczema. I was given a tally counter to log each episode of scratching or touching the skin and this gave me a simple way to track my progress.
I was taught to replace my scratching behaviour with 30 seconds of fist clenching until the urge to scratch subsided. I developed increased awareness of the times I scratched the most and was able to develop creative strategies with Dr Kanji to help minimise this, which have gradually become second nature. Post-shower scratching was habitual. Now, showering is preceded by an organisation of my creams and clothes so that afterwards I can rapidly get dressed, minimising scratching.
I was also taught how to apply my steroids creams and moisturisers effectively. Seeing the number of scratches decrease on a weekly basis gave me confidence that I was making progress and made me feel more optimistic. If this worked, it would mean avoiding powerful drugs in the future.
A few months later, the longstanding eczema was almost completely gone so I no longer needed to start dupilumab injections as was previously planned. I still experience flares of acute eczema, mostly associated with increased levels of stress, but I now have a set of tools that I can combine with the rest of my treatment regime to keep flares of eczema to a minimum.
Find out more
The Eczema Solution, by Sue Armstrong-Brown, is available on Amazon and other bookshops. If you decide to work through the book, consult with your GP or dermatologist.
To find out more about the combined approach and related topics, go to www.atopicskindisease.com.
With thanks to Dr Christopher Bridgett for discussion and feedback on this article.
