We face so many challenges living with eczema. For almost 50 years, National Eczema Society has been working tirelessly to support and champion the needs of people with eczema and their families. We still have have more work to do and we need your support!
Please donate to our Talk Eczema Christmas appeal if you can.
Eczema is complex condition, involving our genetics, immune system, environment and skin barrier. It affects each of us in different ways and there are no simple answers to managing eczema well. This also makes it hard to explain to others what it’s like to live with eczema.
We find ways of coping and getting on with life. We have no choice. The challenges of managing inflamed, painful, cracked skin and the relentless itch are ‘normal’ for too many people. We mostly face these challenges alone, or in silence, but we need to Talk Eczema to help others understand and get better medical care. National Eczema Society wants to give people with eczema a louder voice, by running campaigns and encouraging people to Talk Eczema.
Our charity relies on donations from wonderful supporters like you. Your gift, no matter how big or small, helps to create a better future for people with eczema and their families. It’s quick and easy to donate through our website here. Thank you!
Very best wishes of the season from everyone at National Eczema Society and a happy New Year!
National Eczema Society has worked with other charities to create a Patient Charter for people living with atopic eczema, developed in collaboration with Sanofi. The new Patient Charter is being launched today (6 July 2023) in Westminster, where we are speaking to parliamentarians about the issues that matter to people with eczema.
Most people have heard the name ‘eczema’ and know about some of the more obvious symptoms like skin rash. But it’s hard to appreciate just how devastating eczema can be, unless you or someone close to you has the condition. Eczema is a complex immune-mediated condition that has wide-ranging psychological, social and financial impacts, as well as the more obvious affects on people’s physical health.
From surveys, we know 4 out of 5 people with eczema say the condition has negatively impacted their mental health. Anxiety, depression and suicidal thoughts are much more common amongst people with moderate-to-severe eczema. In a 2021 survey, a third of respondents said they spend at least an hour every day managing their condition, doing things like applying emollients and other topical treatments. Half of the adults who took part in the survey reported having to take time off work because of their eczema.
Our patient charter makes a number of key recommendations:
- Improved access to specialist dermatology care and psychodermatology services
- People living with eczema to become genuine partners with healthcare professionals in their own care
- Better education to help people self-manage eczema and improved mental health support
- Dermatology services are supported to provide patient-centric care.
You can read the patient charter here, which has the full text of our vision for better care for people living with atopic eczema.
National Eczema Society is excited to be co-funding the 2023 UK Dermatology Clinical Trials Network research awards. These are focusing on projects to improve care for people of colour. The Society is awarding a £10,000 grant for the best research proposal to help make life better for people of colour who have eczema. This is in addition to the UK DCTN research award for any aspect of dermatology in skin of colour.
Applications can include work related to outcome measures and pilot or feasibility work, including surveys and qualitative research methods. Please consider applying! The closing date is 17 July 2023.
More information here.
CAMPAIGN UPDATE – May 2024
Our campaign for better labelling of steroid creams and ointments has been successful! National Eczema Society is delighted the UK medicines regulator, the MHRA announced in May 2024 that potency (strength) labelling will be introduced. The new labelling will be added to topical steroid packaging over the coming year. It will show whether the topical steroid is mild, moderate, strong or very strong.
This labelling change is important to help our community use these widely-prescribed medicines safely and effectively. Topical steroids are used by millions of children and adults in the UK to manage eczema flare-ups. We are very grateful to all the patients, healthcare professionals and organisations who supported this important campaign. We also applaud the MHRA for implementing.
May 2023
Leading professional dermatology organisations and other charities have joined National Eczema Society in calling for clear potency (strength) labelling of steroid creams and ointments. We are asking the UK medicines regulator, the MHRA, to ensure pharmaceutical manufacturers include consistent and clear potency labelling on topical steroid (TCS) tubes, packaging and patient information leaflets. Here is the full letter submitted to the MHRA.
Topical steroids are used by millions of adults and children in the UK to treat or prevent eczema flare-ups. It is important patients and their carers have the right information to use these medicines safely and effectively to manage eczema well. Topical steroids are effective treatments for eczema but, like many treatments, they can have side effects. People with eczema and carers are understandably concerned about overusing TCS. We believe clear potency labelling will help improve patient understanding and confidence in these widely-used medicines.
Steroid creams and ointments come in four levels of potency: mild, moderate, potent and very potent. When deciding on topical steroid potency, healthcare professionals take into account factors including eczema severity, the age of the person, and the area of the body where the eczema needs treating. People are sometimes prescribed different potency TCS to use on different areas of the body. Over time, patients can amass a number of different topical steroids medicines, with no meaningful information shown on the tube or packaging about their potency or equivalence.
The situation is made more confusing with the various types and many product names of topical steroid creams and ointments. The product packaging shows the percentage of active ingredient, but it’s difficult working out what this means in terms of the steroid strength. For example, 1.0% hydrocortisone is a mild topical steroid, whereas 0.1% betamethasone valerate is potent. There can be a six hundred-fold difference between mild and very potent topical steroids. Patient information leaflets that come with products rarely state the TCS potency level.
At the moment, the system relies too much on healthcare professionals explaining about potency, but there is not always time for this during busy consultations. It also relies on patients understanding and remembering what is said in consultations. We can – and must – do better.
We need standardised labelling, so that patients and healthcare professionals become familiar with the way that potency is shown across all the many different topical steroid products and brands. The labelling scheme must be independent of language and literacy level, to be inclusive and effective. The goal is to achieve a level of patient understanding comparable to sunscreen strength using the Sun Protection Factor (SPF) labelling, which enables people to use sunscreens confidently and effectively.
This call for clearer labelling has strong support from the eczema community. National Eczema Society conducted an online survey in January this year, to find out more about people’s knowledge and understanding of steroid potency. We received 943 responses, from both adults with eczema and parents of children with eczema, and many thanks to everyone in the eczema community who took part.
Almost all respondents, some 98%, knew that TCS comes in different potences (strengths). However, almost half said they did not know how many different strengths there were, and only 17% correctly answered ‘4’. Most people (70% of respondents) said they would look at information printed on the tube or product packaging to find out about potency. It seems a glaring omission that potency information is not routinely provided at the moment. Some 95% of respondents said they would like to see clear strength labelling on all steroid creams and ointments. See here for the full survey results.
A report on the findings from this survey, and a further survey conducted in March investigating awareness of specific topical steroid products, has been published in the Clinical and Experimental Dermatology Journal – see here. The research highlights a worrying lack of understanding of steroid potency among patients. 1 in 5 respondents underestimated the potency of their topical steroid and almost a quarter overestimated this. Many people used the survey to express their concerns with topcial steroids.
This initiative for clearer labelling has strong support from healthcare professionals and other charities, with the following organisations endorsing the National Eczema Society’s campaign:
- British Association of Dermatologists
- British Dermatological Nursing Group
- British Society for Paediatric and Adolescent Dermatology
- British Society for Allergy & Clinical Immunology
- Dermatology Council for England
- Eczema Outreach Support
- Primary Care Dermatology Society
- Scottish Dermatological Society
Please see our webpage and other information for more about topical steroid treatments for eczema.
The survey is now closed – thank you everyone who took part.
Do you use steroid creams and ointments to manage eczema flare-ups? If you do, please consider completing our short online survey.
Topical steroids are used routinely to treat skin conditions including eczema. Some products can be purchased in pharmacies and others are prescribed by healthcare professionals. It’s important people know the strength of their topical steroids, to use them safely and effectively for maximum benefit.
National Eczema Society wants to learn more about people’s understanding of steroid creams and ointments. If you live in the UK and have eczema, or care for children with eczema, please complete our online survey. It only takes a few minutes. The results will provide valuable new evidence about people’s knowledge of these commonly-used medicines. They will also highlight areas where we need to improve understanding. Thank you!
Email us at info@eczema.org if you want more information about the survey, or information about topical steroid treatment for eczema. You can read our factsheet on Topical steroids here.
New study finds low treatment satisfaction, poor control of eczema symptoms, high psychosocial burden and clear gaps in patient-centered care for eczema patients worldwide.
The Global Patient Initiative to Improve Eczema Care (GPIIEC), a partnership of eleven patient organizations, today (6 April 2022) released a global report of eczema patient care in eight countries: Australia, Canada, Denmark, France, Italy, Germany, United States, and the United Kingdom. National Eczema Society contributed views and experiences of people with eczema from the UK.
The Initiative is a global collaboration to establish common measures to assess the responsiveness of health systems to the needs of patients and their caregivers, and to identify opportunities for improvement.
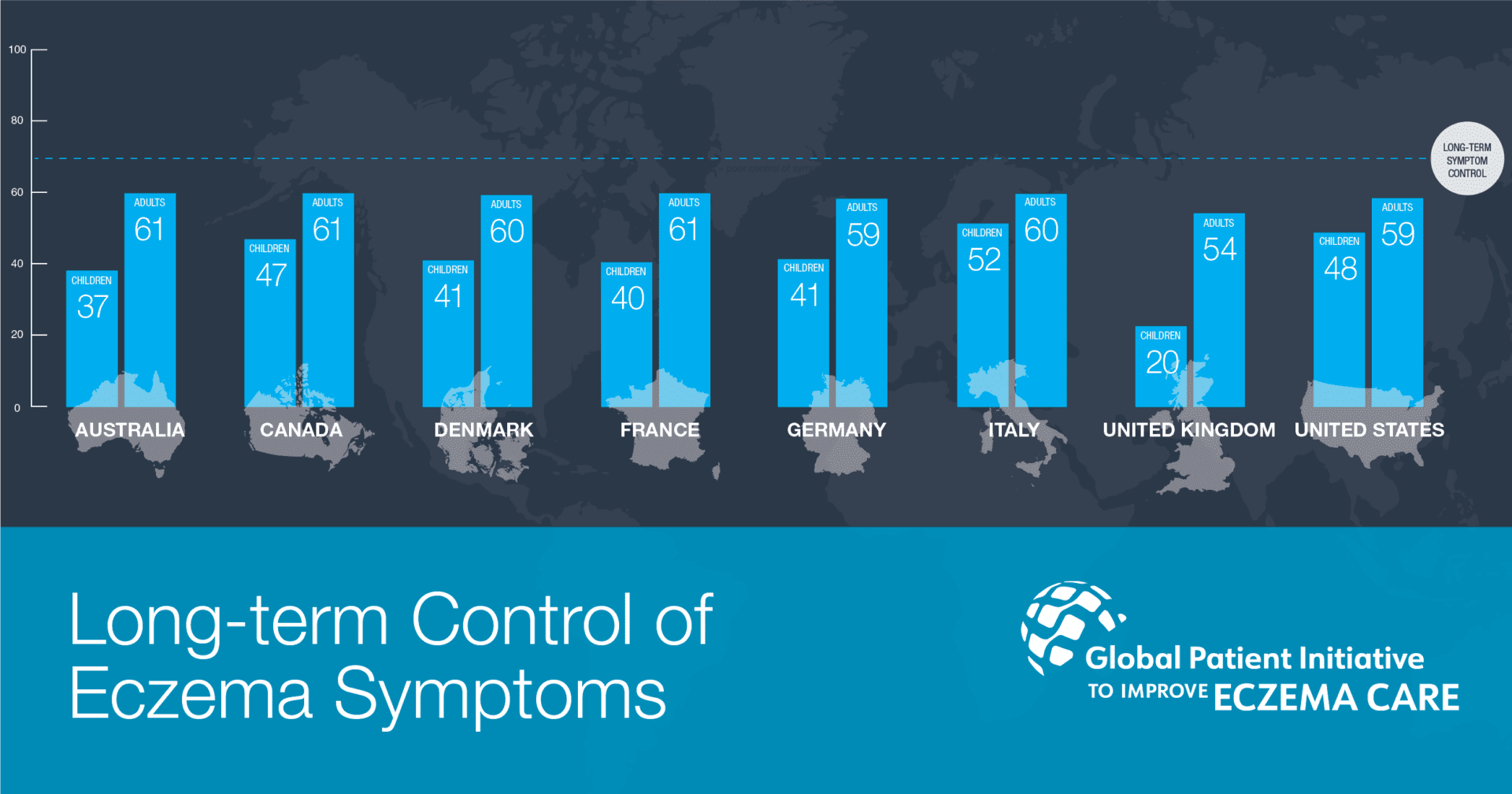
Eczema is a long-term relapsing inflammatory skin condition that impacts approximately 15% to 20% of children and 1% to 3% of adults globally, resulting in a significant patient burden and high demand on health care systems. A global survey by the GPIIEC that received over 3,000 responses found that patients in every country, and particularly those who lived with moderate to severe eczema, are struggling to achieve long-term control of their eczema symptoms and report limited satisfaction with current treatments.
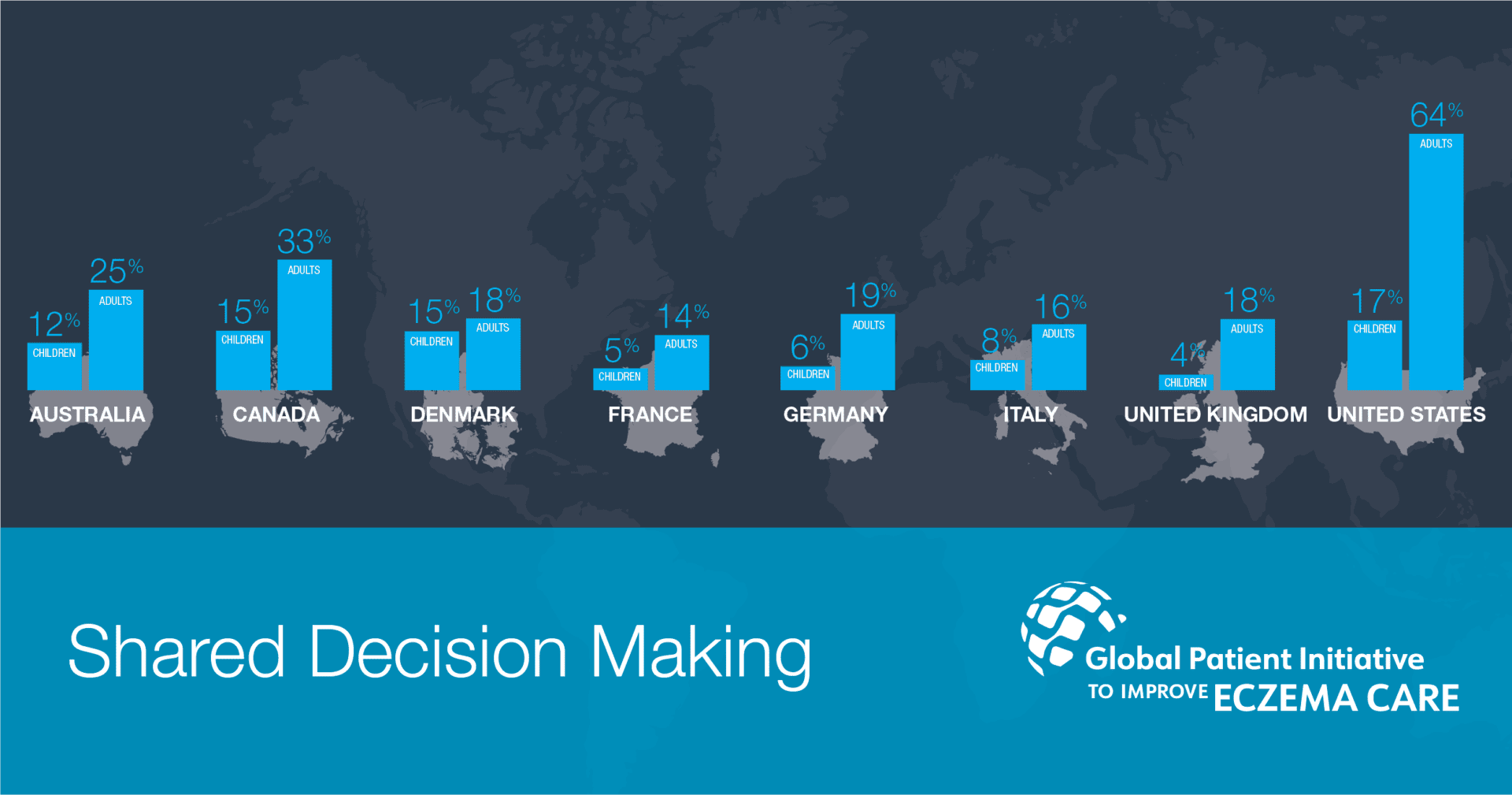
Survey respondents from the UK, both adults and parents of children with eczema, reported the lowest or low scores on the measures for long-term control of eczema symptoms, satisfaction with eczema treatments, patient education, shared decision making and life span trade-off.
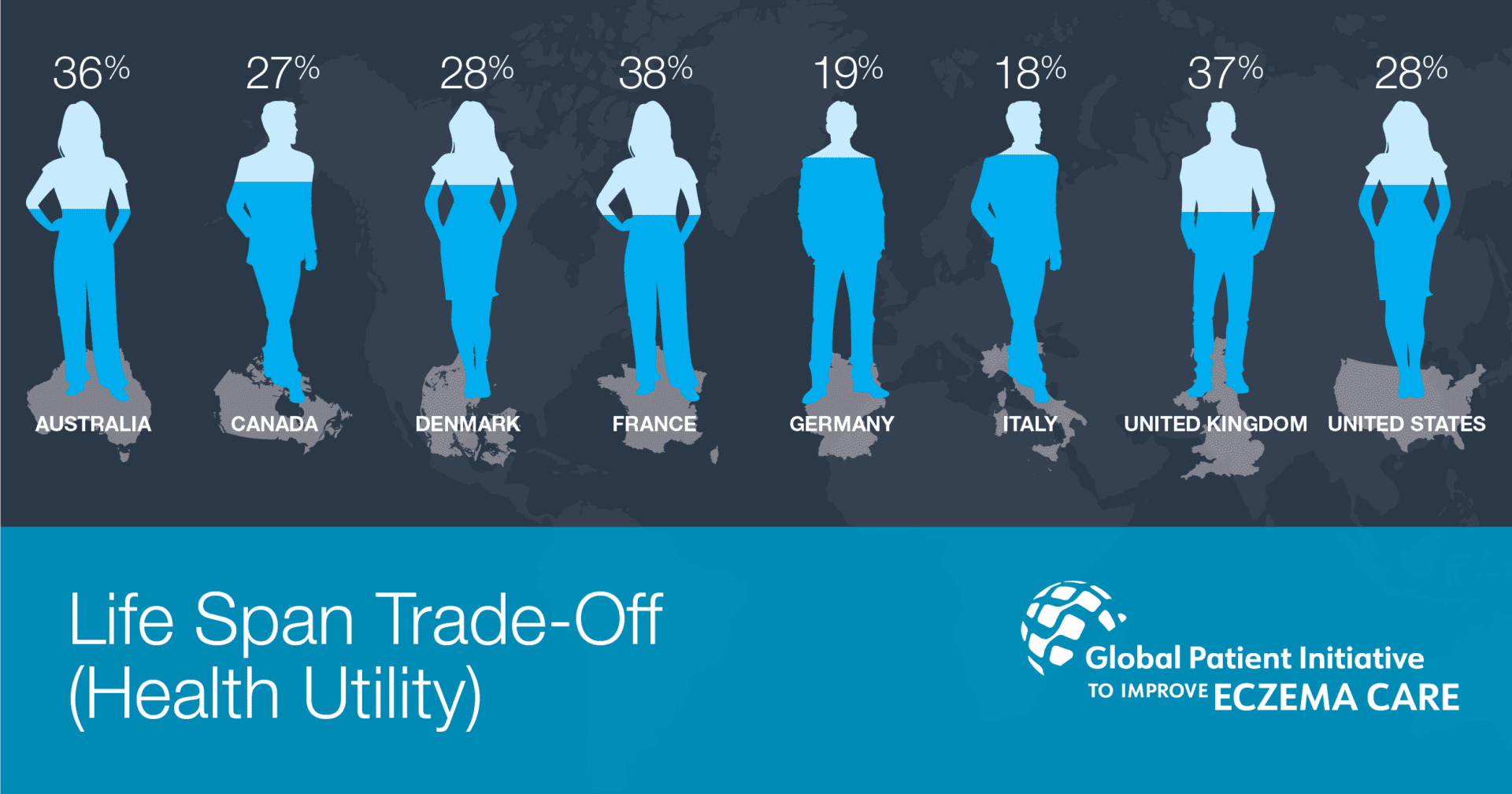
Poorly controlled eczema, which does not respond well to current treatments, has a substantial impact on patients’ health-related quality of life. Based on adult patients’ descriptions of their health, they would be willing to sacrifice between 18-38% of their remaining life span in order to be restored to perfect health. Key drivers of lower quality of life were the pain and discomfort of eczema and the mental health impacts such as anxiety and depression.
Moderate to severe eczema is complex and chronic, demanding a high degree of patient involvement in ongoing symptom management. However, education and training for this role is minimal and patient input into treatment decisions is lacking in almost every country surveyed. Interestingly, shared decision making, defined as asking patients and caregivers about their priorities during a medical visit, was predictive of symptom control. This finding suggests that such involvement may improve medical care and outcomes, and serves as a target for improvement for health systems in each country.
About Global Patient Initiative to Improve Eczema Care (GPIIEC)
GPIIEC is a patient organization-led effort to measure the performance of health systems in meeting the needs of people with eczema (atopic dermatitis) and their caregivers using a common methodology to allow for direct comparisons. For more information: www.improveeczemacare.org
