Wednesday 3 May, 6:00-7:00pm
This event has now taken place – you can see a recording of the webinar on National Eczema Society’s Facebook page.
This free webinar features two informative talks from dermatology experts at the forefront of eczema research and practice. We will explore the new systemic treatments for people with more severe eczema and how they work, including biologic and JAK-inhibitor medicines. We will also look at how research is helping us understand more about how systemic eczema treatments work, and highlight a new research study called BEACON. This study is looking to compare the effectiveness of different eczema treatments. National Eczema Society and St John’s Derm Academy are pleased to collaborate to bring you this free webinar. There will be time after the talks for you to ask questions of the speakers and panel.
The webinar will be livestreamed via Facebook and the recording will remain available to watch afterwards – see here. To able to participate in the webinar, you would need to register in advance.
6:00pm Welcome and overview of the evening
Professor Catherine Smith
6:05pm What are the new systemic treatments for severe eczema and how do we know how good they really are?
Dr Andrew Pink
6:25pm Understanding how systemic eczema treatments work
Dr Satveer Mahil
6:45pm Question and answer session with a panel including webinar speakers, plus Professor Catherine Smith and Andrew Proctor, Chief Executive of National Eczema Society. Participants are encouraged to ask questions on the topics being presented, as well as other areas of eczema care.
7:00pm Close
Webinar speakers and panel
Professor Catherine Smith
Consultant Dermatologist, St John’s Institute of Dermatology
Guy’s and St Thomas’ NHS Foundation Trust, London
Professor Smith is Consultant Dermatologist and Professor of Dermatology and Therapeutics at St John’s Institute of Dermatology, Kings College London and Guys and St Thomas’ Hospital. She is lead clinician in national specialised services for adults with severe eczema. Her clinical and research interests focus on inflammatory skin disease and translational medicine, extending from biomarker discovery through to interventional studies (phase II-IV), and involve major national and international collaboration. These include BIOMAP, a European-wide consortium focussed on identifying clinically relevant biomarkers in atopic eczema and psoriasis https://biomap-imi.eu/ and BEACON – a UK wide platform trial of systemic interventions in adult eczema https://www.beacontrial.org/.

Dr Andrew Pink
Consultant Dermatologist and Director of Adult Clinical Trials Unit
St John’s Institute of Dermatology, Guy’s and St Thomas’ NHS Foundation Trust
Honorary Senior Clinical Lecturer, King’s College London
Dr Pink is a consultant dermatologist and the Director of the adult Clinical Trials Unit at St John’s Institute of Dermatology, Guy’s and St Thomas’ Hospitals, London. He is an Honorary Senior Clinical Lecturer at King’s College London, ex-Honorary Secretary of the St John’s Dermatological Society, a member of the International Psoriasis Council, Chair of the Annual UK Dermatology Course for Consultants and regularly acts as a NICE clinical expert. His clinical and academic interests focus on inflammatory skin disease and translational medicine, primarily in eczema and psoriasis. Andrew has helped to develop a national multi-disciplinary eczema service and a very active trials unit (phase II-IV) at St. John’s. He has acted as CI on multiple trials examining novel therapies emerging in psoriasis and eczema and is the Chief Investigator for the BEACON trial, a large UK platform trial designed to assess the comparative effectiveness of systemic therapies for moderate to severe eczema in adults.

Dr Satveer Mahil
Consultant Dermatologist
St John’s Institute of Dermatology
Guy’s and St Thomas’ NHS Foundation Trust
Dr Mahil is a Consultant Dermatologist at Guy’s and St Thomas’ Hospital. She qualified from Cambridge University and completed integrated academic training (NIHR Academic Clinical Fellowship and NIHR Clinical Lectureship) in dermatology at St John’s. She completed a MRC-funded PhD in 2017, during which she used genetic information to gain novel insights into the mechanistic basis of different forms of psoriasis, and define new therapeutic targets.
Alongside her clinical and education work at St John’s, she continues to conduct translational research, which is focused on optimising outcomes for individuals with inflammatory skin diseases.

Andrew Proctor
Chief Executive of National Eczema Society
Andrew joined National Eczema Society as Chief Executive in March 2018. He has worked in the voluntary sector for over 15 years, including spells with Asthma UK, Alzheimer’s Society and Action Medical Research. He believes passionately in people having the right information and advice to make informed choices about their health, and in supporting people to self-manage their health conditions effectively. Andrew has a particular interest in digital, which he sees as playing an increasingly important role in healthcare and in helping National Eczema Society reach more people affected by eczema. He is inspired by the Society’s many members, donors, partners and other stakeholders who work so hard to improve the quality of life for people with eczema.
The skin of many people with eczema improves in the spring and summer months. This is often due to the effects of natural sunlight – although it’s still important to protect the skin from harmful rays!
Where sunscreens are concerned, we recommend trying an unfragranced, broad-spectrum (UVA and UVB protector), mineral-based sunscreen. Sunscreens can be divided into organic (chemical) UV absorbers or inorganic (mineral-based, i.e. containing titanium dioxide or zinc oxide) UV reflectors. Many people with eczema find that mineral-based sunscreens are less irritating to their skin than chemical absorbers. For more sunscreen information, please see our Sun and eczema page.
Different types of pollen can cause problems for people at different times of the year. Tree pollen season tends to be from March to May. Common symptoms of pollen allergy are a runny nose, sneezing and swollen eyes – known as allergic rhinitis or hay fever. Most people with atopic eczema find that their skin is not really affected by the pollen season. If your skin is affected, here are some tips:
- Limit exposure on days where the pollen count is high by staying indoors and steering clear of known allergens when you can.
- Always have your eczema treatments readily available (take them with you when you go out) as tackling a flare-up quickly is imperative.
- You may also need to take an oral antihistamine (medication that helps suppress the body’s release of histamine in response to an allergen). The ‘non-drowsy’ kind can be helpful in relieving the symptoms of allergy throughout the body, including the eyes, nose and skin. The sedating antihistamine can also be useful in helping to prevent night-time scratching.
- If you’ve been doing something outdoors that might have brought you into contact with pollen, then a shower and change of clothes will remove any pollen particles you’ve inadvertently attracted.
- If you have pets, pollen is easily transmitted into the home and onto your skin via their fur. Cleaning and brushing their coats – or better still, asking someone who does not suffer from allergy to do this! – and banishing your furry friends from certain rooms, is therefore a good idea.
You’re invited to a talk organised by the West Surrey and North East Hants Support Group of National Eczema Society at 2pm on Saturday 4 March.
This event has now taken place, and you can view the recording on Facebook.
Join the West Surrey and North East Hants Support Group of National Eczema Society for an Information Afternoon, where Professor Sinéad Langan, Professor of Clinical Epidemiology and Wellcome Senior Clinical Fellow at the London School of Hygiene and Tropical Medicine, will be delivering a talk and answering questions. In a study examining the health records of more than 3 million adults, there is evidence of a strong link between atopic eczema and the risk of bone fractures and cardiovascular disease.
Attend in person at The Pavilion, Woodbridge Road, Guildford GU1 4RP
Or join via our Facebook livestream, here. You don’t need a Facebook account to watch the livestream.
Eczema is a common skin condition, affecting 1 in 5 children and up to 1 in 10 adults in the UK, and is becoming more common globally. Symptoms include intense itch, pain, sleeplessness and low self-esteem.
Entry is free but donations are very welcome. National Eczema Society literature will be available.
The survey is now closed – thank you everyone who took part.
Do you use steroid creams and ointments to manage eczema flare-ups? If you do, please consider completing our short online survey.
Topical steroids are used routinely to treat skin conditions including eczema. Some products can be purchased in pharmacies and others are prescribed by healthcare professionals. It’s important people know the strength of their topical steroids, to use them safely and effectively for maximum benefit.
National Eczema Society wants to learn more about people’s understanding of steroid creams and ointments. If you live in the UK and have eczema, or care for children with eczema, please complete our online survey. It only takes a few minutes. The results will provide valuable new evidence about people’s knowledge of these commonly-used medicines. They will also highlight areas where we need to improve understanding. Thank you!
Email us at info@eczema.org if you want more information about the survey, or information about topical steroid treatment for eczema. You can read our factsheet on Topical steroids here.
Mpox (previously known as Monkeypox) is a rare infection that appears on the skin as raised spots, which turn into small blisters filled with fluid. These blisters eventually form scabs, which later fall off. The skin symptoms of mpox have the potential to be confused with infected eczema, particularly eczema herpeticum, which is a serious viral herpes infection. For more information on the other symptoms of mpox, which appear before the skin symptoms, please see the NHS website. For more information on eczema herpeticum, please see this page.
Children and adolescents with a history or presence of atopic eczema are at risk of more severe mpox. If you suspect that you or your child has mpox – or eczema herpeticum – please seek immediate same day medical advice.
Mpox vaccine (MVA-BN) and cautions for people with eczema
The vaccine recommended to protect against mpox is a third generation Modified Vaccinia Ankara (MVA) vaccine, which was first developed in the 1950s for the prevention of smallpox. See the UK Health Security Agency (UKHSA) website for more information. For most people, the mpox vaccine has a favourable safety profile.
People with atopic eczema, though, may be more likely to experience certain side effects from the vaccine. These include more intense local skin reactions (such as the skin becoming red or darker than usual, depending on skin tone, swelling and itching) and other general symptoms (such as headache, muscle pain, feeling sick or tired), as well as a flare-up or worsening of their eczema. In rare cases, people with atopic eczema have experienced serious reactions to the vaccine with widespread infection of the skin.
National Eczema Society and the UKHSA recommend that people with atopic eczema seek a risk assessment before taking the vaccine in order to balance the risk from exposure to mpox and the risk of possible side effects from vaccination.
The MVA vaccine is currently being offered to people in the UK at high risk of exposure to mpox. Note there have been challenges reported in obtaining sufficient supplies of the vaccine (as of August 2022). The UKHSA recommends MVA is offered to:
- healthcare workers caring for patients with confirmed or suspected mpox
- men who are gay, bisexual or have sex with other men, and who have multiple partners, participate in group sex or attend sex on premises venues. Staff who work in these premises may also be eligible
- people who have been in close contact with someone who has mpox – ideally they should have the vaccine within 4 days of contact, but it can be given up to 14 days after.
References
- NHS webpage on mpox: https://www.nhs.uk/conditions/monkeypox/
- National Eczema Society webpage describing eczema herpeticum: https://eczema.org/information-and-advice/living-with-eczema/skin-infections-and-eczema/
- UKHSA vaccination information: https://www.gov.uk/government/publications/monkeypox-vaccination-resources/monkeypox-waiting-for-your-vaccination
- UKHSA information on the smallpox (MVA) vaccination: https://www.gov.uk/government/publications/monkeypox-vaccination-resources/protecting-you-from-monkeypox-information-on-the-smallpox-vaccination
- UKHSA recommendations for the use of pre and post exposure vaccination during a mpox incident: https://www.gov.uk/government/publications/monkeypox-vaccination
New study finds low treatment satisfaction, poor control of eczema symptoms, high psychosocial burden and clear gaps in patient-centered care for eczema patients worldwide.
The Global Patient Initiative to Improve Eczema Care (GPIIEC), a partnership of eleven patient organizations, today (6 April 2022) released a global report of eczema patient care in eight countries: Australia, Canada, Denmark, France, Italy, Germany, United States, and the United Kingdom. National Eczema Society contributed views and experiences of people with eczema from the UK.
The Initiative is a global collaboration to establish common measures to assess the responsiveness of health systems to the needs of patients and their caregivers, and to identify opportunities for improvement.
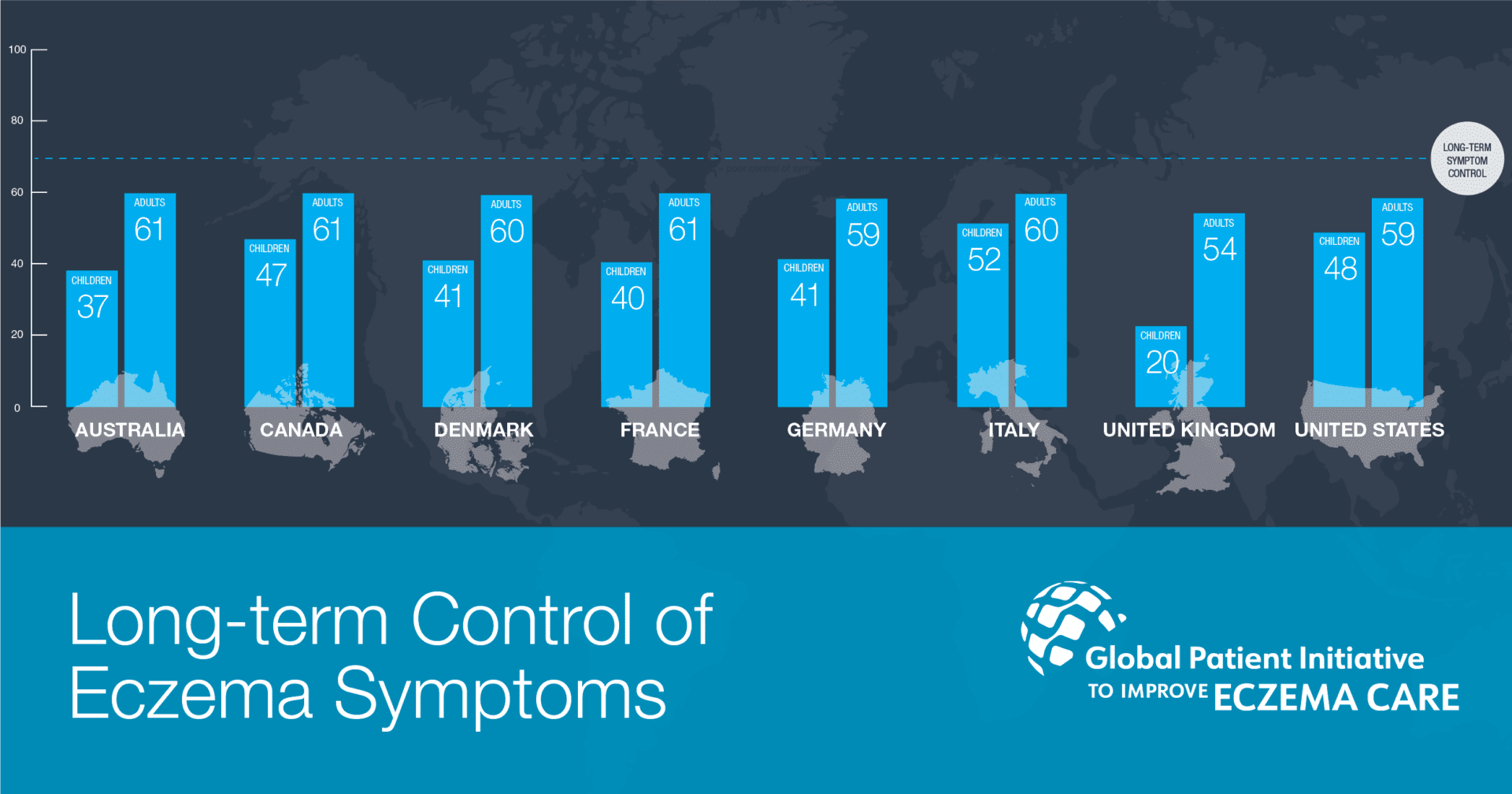
Eczema is a long-term relapsing inflammatory skin condition that impacts approximately 15% to 20% of children and 1% to 3% of adults globally, resulting in a significant patient burden and high demand on health care systems. A global survey by the GPIIEC that received over 3,000 responses found that patients in every country, and particularly those who lived with moderate to severe eczema, are struggling to achieve long-term control of their eczema symptoms and report limited satisfaction with current treatments.
Survey respondents from the UK, both adults and parents of children with eczema, reported the lowest or low scores on the measures for long-term control of eczema symptoms, satisfaction with eczema treatments, patient education, shared decision making and life span trade-off.
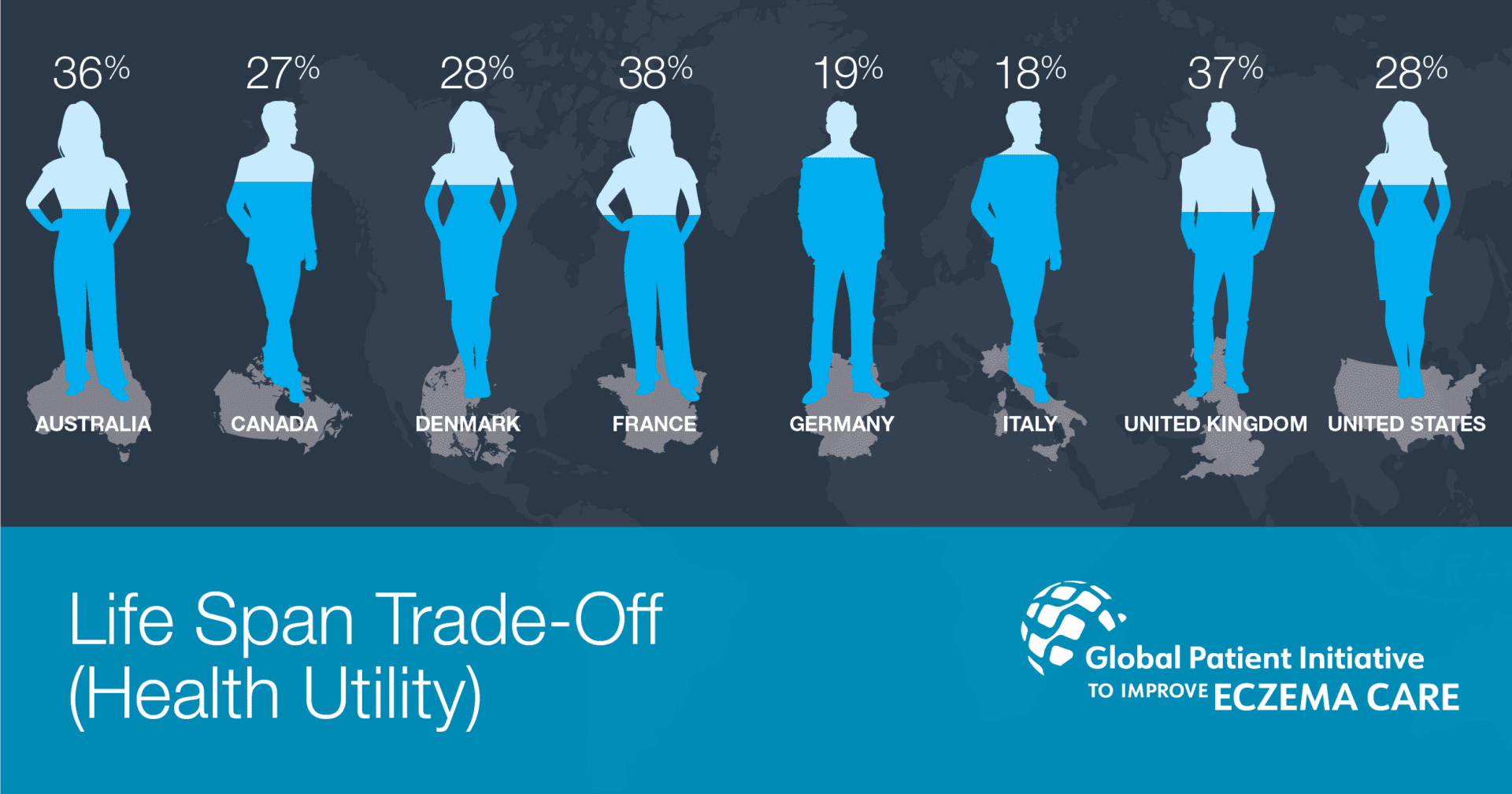
Poorly controlled eczema, which does not respond well to current treatments, has a substantial impact on patients’ health-related quality of life. Based on adult patients’ descriptions of their health, they would be willing to sacrifice between 18-38% of their remaining life span in order to be restored to perfect health. Key drivers of lower quality of life were the pain and discomfort of eczema and the mental health impacts such as anxiety and depression.
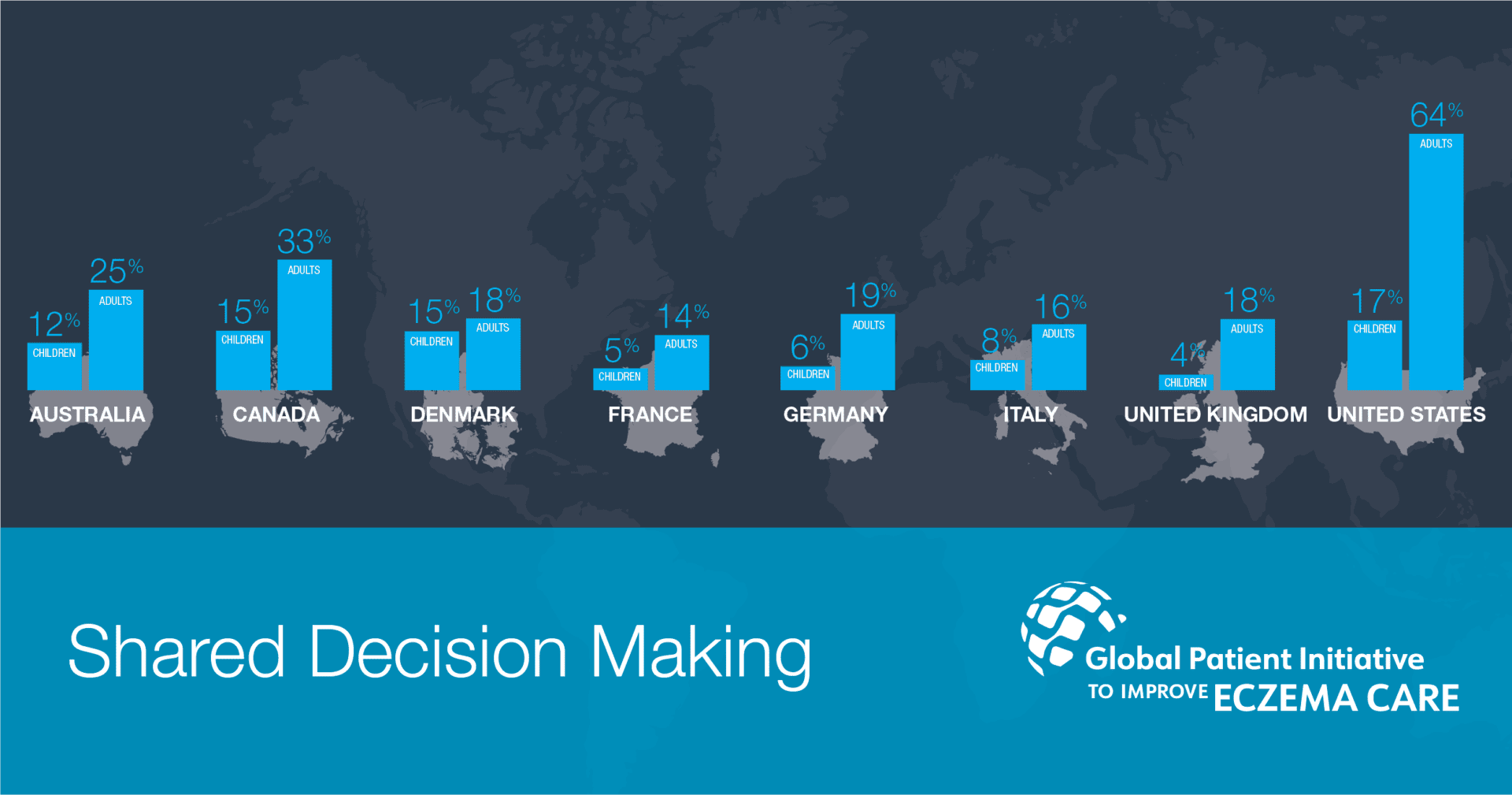
Moderate to severe eczema is complex and chronic, demanding a high degree of patient involvement in ongoing symptom management. However, education and training for this role is minimal and patient input into treatment decisions is lacking in almost every country surveyed. Interestingly, shared decision making, defined as asking patients and caregivers about their priorities during a medical visit, was predictive of symptom control. This finding suggests that such involvement may improve medical care and outcomes, and serves as a target for improvement for health systems in each country.
About Global Patient Initiative to Improve Eczema Care (GPIIEC)
GPIIEC is a patient organization-led effort to measure the performance of health systems in meeting the needs of people with eczema (atopic dermatitis) and their caregivers using a common methodology to allow for direct comparisons. For more information: www.improveeczemacare.org
